
Your PSA Level is High… Now What?
Chances are, you’ve heard the acronym “PSA.” It stands for prostate-specific antigen, a protein produced by cells in the prostate, which is a walnut-sized gland below the bladder that’s involved...
Read Article
Early Detection. A Breadth of Options
Georgia Urology is dedicated to delivering the highest quality of care to men with prostate cancer. We work to help each patient understand their risk factors, detect the disease early at its most treatable stage, and provide an integrated system of care so that they can beat prostate cancer and continue living their fullest life.

It is rare for patients to present because of symptoms attributable to prostate cancer. Most prostate cancers are diagnosed in the local stage and are asymptomatic.
Since the prostate surrounds your urethra, any change in your prostate can cause problems with urination and ejaculation. These symptoms can also be caused by other diseases or disorders which are not caused by prostate cancer. Please consult your urologist to determine their cause.
Because prostate cancer often has no symptoms, the American Urological Association (AUA) recommends that men talk to their doctors about screening starting at age 40. Prostate cancer screening consists of 2 simple and quick tests:
Prostate Specific Antigen (PSA) is a protein produced by the prostate, and normally, very small amounts are released into your bloodstream. When prostate cancer is present, excess amounts of PSA are released. This can be easily detected in your blood with a simple blood test. Your PSA can also be elevated by other prostate problems, such as infection or an enlarged prostate. A small amount of prostate cancers do not produce much PSA but present as a nodule or firmness on the prostate. Therefore, a digital rectal exam is also recommended in conjunction with a PSA blood test.
In this test, your physician will examine your prostate through the rectum. This will allow him or her to feel for any irregularities in the size, shape, or texture of your prostate. Nodules or firmness on the prostate may indicate cancer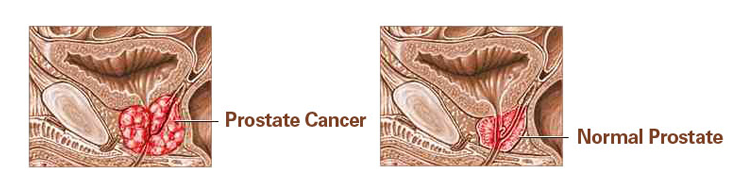

If your screening tests show signs of possible prostate cancer, your doctor will likely refer you to an urologist. The urologist may recommend a prostate biopsy. Using an ultrasound, the urologist will take small biopsies of the prostate to determine if prostate cancer is present.

The earlier prostate cancer is detected, the more treatment options will be available to you. Based on the prostate cancer grade and stage, your age, overall health status, and personal lifestyle, your urologist will discuss treatment options with you. Some prostate cancers do not even need to be initially treated and can be safely monitored for an extended period.
For prostate cancers requiring treatment, the most common forms of treatment are surgery to remove the prostate and radiation directed at the prostate.
Patient TestimonialMen in the early stages of prostate cancer, with slow-growing disease, or those with advanced age or serious diseases may be advised to monitor the prostate cancer rather than actively treat it. For these men, this risk of prostate cancer growing or spreading is very low compared to the risks of side effects associated with treatment.
NanoKnife is an innovative, minimally invasive treatment option that uses non-thermal energy to create tiny pores in the protective barrier of the cancer cell, which causes cell death. Learn more about NanoKnife.
HIFU is a treatment that uses high-frequency sound waves to destroy prostate cancer cells. The waves create heat that destroys the cancer cells. Learn more about High Intensity Focused Ultrasound (HIFU).
High-energy rays or particles of radiation are used to kill cancer cells either by external beam or internal implantation (brachytherapy). Georgia Urology offers SpaceOAR to help relieve complications during prostate radiation therapy.
Hormone therapy is used in certain cases to reduce the levels of male hormones in the body which can make prostate cancer shrink or grow more slowly.
Chemotherapy is used in cases of advanced disease or if the cancer is not responding to other therapy.
An outpatient procedure, performed while the patient is under anesthesia, in which tiny, radioactive seeds are placed inside the prostate gland to attack the cancer.
Cryotherapy is typically used as a treatment when prior radiation therapy has failed. It is an outpatient procedure done under anesthesia where the prostate cancer is killed by freezing the prostate. This procedure is very well tolerated with few side effects.
Immunotherapy is a treatment that is designed to help the immune system (the body’s natural defense) fight disease. The immune system is made up of immune cells found in the body. These cells work as the body’s natural defense against all types of illness, including prostate cancer. PROVENGE is the only FDA-approved treatment that uses the body’s immune system to fight prostate cancer.
A radical prostatectomy is a surgical procedure that removes the cancerous prostate gland. The highly skilled and experienced urologists at Georgia Urology utilize the most advanced techniques to reduce side effects and surgical complications. One such technique is the state-of-the-art Da Vinci robotic surgical system which many of our urologists at hospitals throughout metro Atlanta use to perform a radical prostatectomy. A robotic-assisted prostatectomy allows precise surgical removal of the prostate while preserving important structures for urinary control and sexual function. Dr. Sharpe saw a 70-year-old patient who underwent a prostatectomy treatment at Georgia Urology.

Advanced prostate cancer is when cancer spreads to areas outside of the prostate gland, such as bones, lymph nodes, or nearby tissue. While there is currently no cure for Advanced Prostate Cancer, different treatments can vastly expand the length of life and mitigate symptoms.
You are at a higher risk for prostate cancer if:

For information on dosage, administration, side effects, and more on medications used in the treatment of advanced prostate cancer:

Chances are, you’ve heard the acronym “PSA.” It stands for prostate-specific antigen, a protein produced by cells in the prostate, which is a walnut-sized gland below the bladder that’s involved...
Read Article
What we eat impacts every physiological process and anatomical structure, and the prostate is no exception. The foods we consume directly affect how the prostate functions. Lycopene has been on...
Read ArticleIs Low-Dose Daily Cialis/Tadalafil Effective in Treating Erectile Dysfunction/ED?
Cialis (Tadalafil) is best known as a treatment for erectile dysfunction, but it is also approved for benign prostatic hyperplasia...Read
Can Your Habits Help Prevent Bladder Cancer… Even if It Runs in the Family?
Bladder cancer doesn’t get as much airtime as other cancers, but it should. It’s the 10th most common cancer worldwide,...Read